An Uncommon Presentation: Mandibular Metastasis from Colon Cancer
The case of mandibular metastasis from colorectal cancer is one that truly exemplifies the tricky parts of modern oncology. While colon cancer is one of the most common cancers in the world, its spread to the jaw is a rare and nerve-racking phenomenon. In this opinion editorial, we take a closer look at this unusual presentation, exploring how a primary colon tumor can manifest as isolated jaw pain and the many tangled issues that clinicians face during diagnosis and treatment.
When a patient presents with jaw pain, it is usually easy to chalk it up to dental infections or other benign conditions. However, in rare cases, persistent discomfort may be a sign of deeper, more complicated pieces—like metastatic cancer. A recent case study involving a 57-year-old male patient highlighted the importance of considering these off-the-beaten-track diagnoses, particularly when the primary cancer is silent.
Understanding the Spread: How Colon Cancer Reaches the Jaw
Colorectal cancer (CRC) typically disseminates to the liver, lungs, peritoneum, or lymph nodes. The occurrence of osseous metastases is less common, and involvement of the mandible is even more so. The journey of tumor cells from the colon to the jaw involves many subtle parts that researchers and clinicians must get into. The process is driven by hematogenous spread, in which circulating tumor cells find their way into the richly vascularized bone marrow of the jaw.
Some of the small distinctions that make this pathway unique include:
- The jawbone’s high vascularity, especially in the molar area, providing an unlikely home for disseminated cells.
- A delay in diagnosis due to the deceptive similarity of symptoms between metastatic pain and common dental issues.
- The additional risk of mistaking these lesions for benign or inflammatory conditions instead of quickly identifying them as life-threatening.
Given these slight differences, it becomes clear why timely detection is super important. Physicians must take a closer look when patients, particularly those in their late 50s to 70s, experience persistent jaw pain along with other vague gastrointestinal symptoms or a history of altered bowel habits.
Oral Metastasis Diagnostic Challenges
Oral metastasis is a subject that is both intriguing and full of problems. It adds yet another layer of complexity to an already intimidating process of cancer diagnosis. The diagnostic workup involves several steps—from clinical assessment and imaging studies to biopsy and immunohistochemical analysis. Each step can present its own confusing bits and nerve-racking twists and turns.
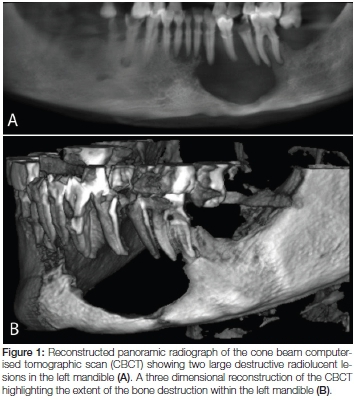
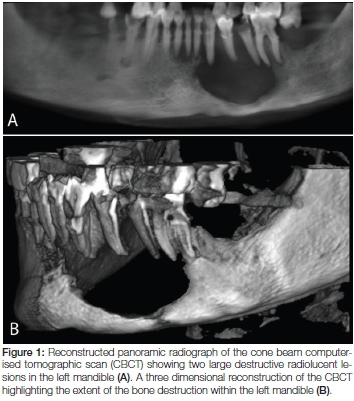
Imaging: Uncovering Hidden Lesions
Imaging studies, such as computed tomography (CT) and magnetic resonance imaging (MRI), are essential when a patient presents with an unusual presentation of jaw pain. In the reported case, a CT scan of the neck revealed a large soft tissue mass with associated bony destruction in the mandibular region. Such images are invaluable in providing a roadmap for further investigative measures. However, in about 5% of cases, these scans may not show any abnormalities, which makes the diagnostic process all the more overwhelming and complicated.
Another imaging tool mentioned in literature is the Technetium-99m bone scan or PET-CT. These methods can be used to detect additional sites of bone metastasis and further assist clinicians in mapping the spread of the disease.
Biopsy and Immunohistochemistry: The Nitty-Gritty Details
Once imaging identifies a suspicious lesion, a biopsy becomes the next essential step. In the case we are discussing, an ultrasound-guided biopsy allowed pathologists to study malignant cells present in the mandibular mass. The results of the histopathological analysis were critical: markers such as cytokeratin AE1/3, CDX2, and SATB2 confirmed the colorectal origin of the metastatic adenocarcinoma.
These immunohistochemical markers represent one of those fine points that help differentiate between various types of cancer. When these markers are expressed in a lesion, they provide strong evidence that the tumor is related to a colorectal primary, rather than arising from local tissues.
Laboratory Investigations: Piecing Together the Puzzle
Laboratory tests also play a role in framing the entire clinical scenario. For example, in the case discussed, the patient’s blood work demonstrated leukocytosis, mild normocytic anemia, and abnormal liver tests. A table summarizing some of these critical lab values might look like this:
| Test | Result | Normal Range |
|---|---|---|
| White Blood Cells (WBCs) | 11,400 /µL | 4,000 – 10,900 /µL |
| Hemoglobin | 12 g/dL | 12 – 16 g/dL |
| AST | 153 IU/L | < 41 IU/L |
| ALT | 109 IU/L | < 54 IU/L |
| Alkaline Phosphatase | 317 IU/L | 38 – 126 IU/L |
| Total Bilirubin | 1.8 mg/dL | 0.2 – 1.2 mg/dL |
These lab results, while not conclusive on their own, contribute to a bigger picture that urges a more detailed investigation, reminding us that even small differences in blood levels can signal larger underlying problems.
Systemic Chemotherapy and the Fight Against Advanced CRC
Once the diagnosis of metastatic colorectal cancer has been confirmed, the treatment strategy shifts towards systemic chemotherapy. This approach is central to managing widespread disease, as aggressive surgical intervention is typically not an option in the presence of extensive metastases.
The FOLFOX Regimen and Its Role in Treatment
The FOLFOX regimen, which combines folinic acid, 5-fluorouracil, and oxaliplatin, plays a key role in the systemic treatment of CRC. In the highlighted case, due to the extent of metastatic disease, surgery was not pursued. Instead, the patient was started on FOLFOX in combination with bevacizumab, an anti-vascular endothelial growth factor (VEGF) agent.
This combination of systemic therapy demonstrated early biochemical and clinical improvement, as evidenced by a notable drop in carcinoembryonic antigen (CEA) levels. Such treatment not only underscores the importance of early diagnosis but also highlights the need for aggressive management of cancer once it has taken a path into unusual, off-target areas like the mandible.
Addressing the Complicated Pieces of Metastatic Treatment
Managing metastatic colorectal cancer is a multifaceted challenge. Some of the key points to consider include:
- Symptom Management: Pain control, especially in the case of bone metastasis, is a must-have consideration. Local radiotherapy, while not curative, can provide significant symptomatic relief for patients facing overwhelming discomfort.
- Quality of Life: Palliative chemotherapy is aimed at relieving symptoms and extending life expectancy, even in the face of a poor prognosis. Balancing the side effects of chemotherapy with its benefits is one of those tricky parts that must be managed with care.
- Multidisciplinary Collaboration: The nature of metastatic disease—particularly when it affects the jaw—calls for close coordination among oncologists, radiologists, pathologists, and palliative care specialists.
These practical points illustrate that while chemotherapy may be a powerful tool, it often comes with its own set of challenges. Early monitoring, such as tracking CEA levels, provides doctors with a gauge to figure a path through treatment adjustments.
Mandibular Metastasis Case Studies: Learning from Experience
The case discussed here is one among fewer than 50 documented instances of metastatic colon cancer to the jaw in the medical literature. Each reported case adds to our collective understanding of the hidden complexities involved in diagnosing and treating such rare presentations.
In many published reports, the jaw metastasis was the first signal of an undiagnosed primary tumor. Often, patients with these atypical presentations share common themes:
- Age Group: Most patients fall within their 60s or 70s, although occasional cases, like the one discussed, involve individuals in their late 50s.
- Gender Predominance: There has been an observed male predominance in these cases.
- Initial Presentation: Jaw pain often precedes any gastrointestinal complaints, which can lead to delays in recognizing the true source of the metastasis.
These observations emphasize the importance of keeping a broad differential diagnosis in mind when faced with jaw pain that does not resolve with standard dental treatments. Sorting out these subtle details early can sometimes make the difference between early intervention and a more advanced, full-of-problems presentation.
Moreover, case studies serve as a reminder that the treatment of oral metastasis is not solely about addressing cancer on a biological level but also about managing the overall quality of life and comfort of the patient. Local therapies, such as radiotherapy, may not extend overall survival, but they can be critical in alleviating pain and improving day‐to‐day functioning, which is key for patient morale.
The Role of Imaging and Biopsy in Identifying Jaw Lesions
The process of identifying jaw lesions, especially when metastasis is a concern, is filled with twists and turns. Radiological imaging and precise histopathological analysis remain two super important tools that aid clinicians in making a definitive diagnosis.
Imaging Techniques: Getting a Closer Look
When the initial clinical presentation is ambiguous, advanced imaging modalities such as CT scans and MRI are deployed to dig into the deeper aspects of the lesion. For example, the CT scan in the discussed case revealed not only a mass in the mandible but also signs of bony destruction, which immediately raised red flags about its malignant potential.
Alongside CT, PET-CT scans and bone scans using Technetium-99m can help map out the full extent of metastatic spread. This comprehensive imaging workup is critical, as it assists doctors in making informed decisions about further diagnostic tests and eventual treatment strategies.
Biopsy: Confirming the Diagnosis
Biopsy remains a cornerstone in the process of confirming metastatic disease. In situations where imaging provides evidence of a destructive process, taking a tissue sample offers the nitty-gritty details needed to pinpoint the origin of the malignancy. In the scenario under review, the biopsy not only confirmed the presence of malignant cells but also revealed the immunohistochemical profile that is characteristic of colorectal cancer.
This detailed analysis, which includes markers like CDX2 and SATB2, plays an essential role in differentiating primary oral tumors from metastatic lesions originating in distant organs. The value of this step cannot be overstated—it is one of the keys to ensuring that patients receive the most appropriate treatment plan.
Challenges and Learning Points: The Broader Implications
One of the most intimidating aspects of dealing with metastatic colorectal cancer that presents in locations such as the jaw lies in its unpredictability. The following points summarize some key learning points drawn from this rare case:
- High Index of Suspicion: Persistent jaw pain in older adults, especially when accompanied by unexplained gastrointestinal symptoms or abnormal lab results, should prompt clinicians to look into unusual causes.
- Importance of a Multidisciplinary Approach: The complex bits of diagnosing and managing metastatic disease require input from a variety of specialties. This collaborative model enhances the probability of early diagnosis and more effective treatment planning.
- Role of Systemic Therapy: When a patient presents with advanced disease—including both mandibular and liver metastases—palliative chemotherapy becomes a mainstay of treatment, with the goal of extending life and improving quality of life even when curative treatment is not feasible.
- Patient Quality of Life: Symptom management, particularly pain control, is a super important aspect of care for patients facing advanced cancer. Even when the prognosis is poor, efforts to relieve suffering are a central part of modern palliative strategies.
These learning points echo the real-world challenges that both patients and clinicians must face together. Each case of atypical metastasis not only broadens our understanding of how cancer can behave but also reinforces the necessity for timely diagnosis and comprehensive care.
Diving Deep into Treatment Strategies for Metastatic CRC
While surgical resection offers potential cure for localized colorectal cancer, the presence of metastatic disease, especially with bone or jaw involvement, shifts the treatment paradigm drastically. Treatment modalities for metastatic CRC are designed to address both systemic spread and local symptoms.
First-Line Systemic Therapies
For most patients with metastatic colorectal cancer, treatment begins with systemic chemotherapy. Regimens like FOLFOX or FOLFIRI (a combination of folinic acid, 5-fluorouracil, and irinotecan) are commonly used in combination with targeted agents. The choice of targeted therapy depends on the molecular profile of the tumor—for example, anti-VEGF agents like bevacizumab or anti-EGFR monoclonal antibodies for those with RAS/RAF wild-type tumors.
The key in selecting these regimens is to balance efficacy with patient tolerance. Many patients may experience side effects related to chemotherapy, so maintaining quality of life is as super important as attempting to control the disease. Regular monitoring through blood tests, including tumor markers like CEA, is essential to assess treatment response and adjust therapy as needed.
Local Therapies: Relieving Jaw-Related Discomfort
Even though systemic therapy remains the cornerstone for metastatic CRC, local treatment approaches play a significant role in managing symptoms. Radiotherapy, though it offers no significant survival benefit, may be deployed to provide relief from intense jaw pain caused by bony involvement. The decision to use such therapies is driven by a careful evaluation of the patient’s overall condition and the risk of side effects.
Other considerations include the use of antiresorptive agents, which can help curb skeletal-related events; however, clinicians must be cautious of potential adverse effects such as osteonecrosis of the jaw. The treatment strategy becomes a balancing act: managing the cancer while also ensuring that the interventions themselves do not add further complications to the patient’s overall health.
Key Considerations in Managing Quality of Life
In the context of metastatic cancer, particularly when it involves areas like the jaw, attention to quality of life is not just an afterthought—it is a fundamental component of patient care. While it may seem scary to confront the reality of a poor prognosis, there are several approaches aimed at easing the patient’s journey.
Palliative Care and Supportive Measures
Palliative care, which focuses on relief from the symptoms and stress of serious illness, is a must-have for patients dealing with advanced metastatic colorectal cancer. The goals of palliative care include:
- Managing chronic pain and providing symptomatic relief.
- Offering emotional and psychological support to both patients and their families.
- Coordinating a multidisciplinary approach to address various health challenges concurrently.
- Ensuring that treatment decisions remain aligned with the patient’s preferences and overall quality of life.
These supportive measures are just as important as aggressive cancer treatments. They help smooth the rough patches of the patient’s experience and create some semblance of control over an otherwise overwhelming disease process.
Monitoring and Follow-Up: Charting Progress
Regular clinical follow-up is essential in evaluating the patient’s response to treatment. Beyond monitoring biochemical markers like CEA, doctors routinely assess the patient’s symptom burden, overall physical health, and mental well-being. This systematic approach assists in finding your way through the ever-changing landscape of metastatic cancer treatment.
Follow-up visits offer an opportunity not only to adjust chemotherapy dosages but also to tweak palliative care strategies. They serve as checkpoints where the healthcare team can re-evaluate the treatment plan based on the patient’s evolving needs and response to therapy.
Pondering on Future Directions and Research
The rarity of cases involving mandibular metastasis from colorectal cancer invites further research into understanding the hidden complexities of how cancer cells travel and colonize unexpected parts of the body. Future research directions might include:
- Exploring Molecular Pathways: Deepening our understanding of the fine points of hematogenous spread to the bone marrow may help uncover targets for early intervention.
- Advancing Imaging Techniques: Enhancing the sensitivity of current imaging modalities, or developing new ones, can aid in the early discovery of small metastases before they cause significant damage.
- Clinical Trials for Targeted Therapy: Investing in clinical trials that focus on metastasis-directed therapies could potentially offer improved outcomes for patients with rare metastatic presentations.
- Integrated Palliative Programs: Developing comprehensive palliative care models that account for the unique challenges of bone metastasis in the jaw is another area ripe for exploration.
These research avenues are crucial for mitigating the overwhelming uncertainty that often clouds the diagnosis and treatment of such unusual presentations. As our understanding of these processes deepens, it may eventually lead to more tailored and effective treatment strategies that help patients not only to live longer but also to enjoy a better quality of life.
Reflections on the Clinical and Emotional Journey
The story of mandibular metastasis from colon cancer is one that touches both the technical and emotional aspects of medicine. For clinicians, it is a stark reminder of the need to keep an open mind when faced with ambiguous symptoms. For patients, it underscores the importance of early medical evaluation and the diligence required in following up on persistent, unexplained symptoms.
In everyday clinical practice, the decision-making process is full of confusing bits and nerve-racking twists and turns. It reinforces that every case is unique and that the journey through diagnosis and treatment is a shared experience, one where teamwork, patient commitment, and clinical expertise all come together. Whether it’s interpreting radiological scans, deciphering laboratory reports, or choosing the right chemotherapy regimen, each small decision plays a critical role in the overall management of the disease.
Moreover, stories like these remind us of the human aspect in medicine—a field where every statistic represents a person fighting against time. While the scientific community continues to make strides in understanding cancer, it is the resilience of patients and the dedication of healthcare professionals that ultimately drive progress.
Conclusion: Charting a Path Through Challenging Terrain
The case of mandibular metastasis arising from colorectal cancer is a vivid example of how cancer can behave in unexpected, off-the-beaten-track ways. This uncommon journey—from a primary colon tumor to a destructive jaw lesion—illustrates the tangled issues that make diagnosis and management such a complicated endeavor.
It is clear that when faced with persistent jaw pain, especially in older adults or those with a history of altered bowel habits, clinicians should not rule out the possibility of metastatic disease. Instead, they should take a closer look at the full clinical picture, including imaging studies, biopsies, and laboratory markers. Left unchecked, these subtle parts of the disease can quickly evolve into a full-blown crisis, making early diagnosis a super important step in the patient’s overall care.
At the same time, the introduction of systemic therapies such as FOLFOX combined with targeted agents like bevacizumab offers hope and tangible benefits, even in the face of extensive metastatic spread. These treatments, while not curative, provide a necessary reprieve from the rapid progression of the disease and contribute significantly to improved quality of life.
In reflecting on these cases, it is clear that there is no one-size-fits-all approach. Each patient’s story is woven from many subtle details—small distinctions in clinical presentation, hidden complexities in diagnostic testing, and the nerve-wracking journey through treatment decisions. The challenge lies in continuously working through these issues with empathy, scientific rigor, and a commitment to improving outcomes.
As medical professionals and members of the broader healthcare community, it is our duty to keep digging into these puzzling scenarios. By piecing together the available evidence, engaging in multidisciplinary dialogue, and remediating challenges as they arise, we help pave the way for a future where even the most atypical cases are recognized early and managed effectively.
While the road from diagnosis to treatment in cases like mandibular metastasis is undeniably full of problems, the resilience of the human spirit and the progress of medical science offer a promising outlook. With continuous research, enhanced diagnostic methods, and comprehensive care plans, we stand a better chance of not just prolonging lives but also ensuring that patients live their remaining days with dignity and as little discomfort as possible.
In conclusion, the intersection of colorectal cancer and mandibular metastasis, though rare, serves as a powerful reminder that medicine is as much an art as it is a science. It challenges us to figure a path through complex clinical scenarios while never losing sight of the human beings behind the numbers. As we take the wheel in managing these challenging cases, each lesson learned not only refines our approach to care but also reinforces our commitment to continuously improve patient outcomes in the face of life’s most daunting challenges.
Originally Post From https://www.cureus.com/articles/401678-mandibular-metastasis-from-colon-cancer-presenting-as-jaw-pain
Read more about this topic at
Mandibular Metastasis as the First Manifestation …
Metastatic Marvel: Unravelling a Rare Case of Mandibular…