Artificial Intelligence in Oncology: Balancing Promising Advances with Patient Concerns
The rapid rise of artificial intelligence (AI) in health care is opening up a world of exciting possibilities in oncology. With every breakthrough and innovation, AI brings both promising opportunities and a set of tricky parts that need careful attention. In the realm of cancer care, the integration of AI is transforming not only administrative workflows but also the way decisions are made, prompting a deep conversation about how best to protect patient trust while embracing novel technologies.
AI’s Role in Enhancing Psychosocial Support for Oncology Patients
As AI technology becomes more commonplace, its application in psychosocial care emerges as a key component of patient support. Recent surveys reveal that opinions among patients and caregivers are evenly split on this matter. On one side, many appreciate the potential of AI to streamline cumbersome administrative tasks, ultimately freeing up valuable face-to-face time with providers. On the opposite side, there is a genuine worry that over-reliance on AI might chip away at the human connection that is so essential in the moments that matter most.
The integration of AI for psychosocial support is far from a one-dimensional solution. It promises to make routine aspects of care more efficient, yet introduces tangled issues regarding how personalized interactions are maintained. This duality in purpose—and the subtle parts that come with any groundbreaking technology—requires the oncology community to think carefully about implementing AI in everyday practices.
Divided Perceptions in AI-Driven Cancer Care
One of the most striking findings from recent surveys conducted by organizations such as the Cancer Support Community is that opinions about AI in cancer care are split down the middle. Approximately 50% of patients and caregivers applaud the innovation, especially when AI is positioned as a tool to enhance decision-making and efficient clinical workflows. The other 50% remain wary, expressing concerns that technology might replace the direct, human-to-human interactions that form the core of compassionate patient care.
Below is a concise list summarizing these perspectives:
- Optimistic Views: Improved workflow, quicker access to information, and the freeing up of clinician time for more direct interaction.
- Skeptical Views: Fears over the dilution of personal care, doubts regarding the reliability of AI-driven advice, and concerns over privacy and security.
This divided viewpoint suggests that while AI’s potential is recognized, its actual benefits and safe usage in oncology may hinge on how well providers can address these tricky parts and maintain the delicate balance between technology and personal connection.
Streamlining Administrative Workflows with AI in Cancer Care
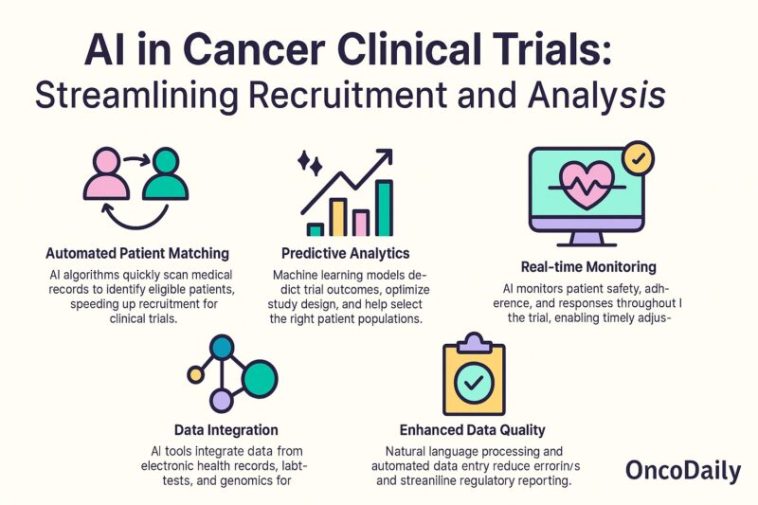
One significant benefit observed in adopting AI is its capacity to digest the fine points of administrative duties that often bog down the clinical process. The implementation of AI tools can help manage data, schedule appointments, and even monitor treatment responses with impressive speed and accuracy.
AI systems are being designed to take on the heavy lifting associated with routine paperwork and scheduling, allowing clinicians to concentrate on tasks that require a human touch—such as discussing treatment options face-to-face with patients. This partnership between technology and careful human oversight is a critical layer that ensures the technology aids rather than detracts from patient care.
Some advantages include:
- Efficient Data Management: AI can sort through vast arrays of patient information quickly, highlighting key findings which facilitate timely decision-making.
- Enhanced Scheduling: Automated systems help coordinate appointments and follow-ups, reducing delays that might otherwise affect treatment timelines.
- Improved Decision Support: By integrating multiple data sources, AI provides clinicians with super important insights that can refine treatment pathways.
These benefits are attractive to both patients and providers as they seek to reduce the nerve-racking burden of administrative overload. However, it remains essential to ensure that such improvements do not come at the expense of personal patient relationships.
Improving Clinical Decision-Making: AI as a Tool, Not a Replacement
Another promising application of AI in oncology centers on its potential to bolster clinical decision-making. By analyzing large datasets and complex treatment outcomes, AI systems offer delicate suggestions that can help clinicians determine the best possible therapeutic strategy.
For instance, AI can weigh a patient’s history, genetic profile, and current health status to suggest personalized treatment pathways—a tool that can be especially useful for complicated cases. However, both patients and caregivers have highlighted that they view these AI recommendations more as an information resource than as definitive medical counsel.
Key points include:
- Personalization of Treatment: AI tools sift through numerous variables to offer a tailored approach to care.
- Decision Support vs. Decision Making: The technology remains a supportive entity rather than the final decision-maker, as clinicians continue to steer the overall treatment plan.
- Assistance with Complex Cases: For situations loaded with issues and subtle differences, AI can help piece together the nitty-gritty needed for more informed choices.
This careful delineation of roles—recognizing AI as an assistant rather than a replacement—helps to alleviate some of the concerns about the technology making health care decisions independently. Patients need clarity on who is at the helm, ensuring that human oversight remains intact.
Ensuring Data Privacy and Security in AI-Enabled Oncology Tools
Privacy remains a hot-topic issue, not just in the realm of health care but across many industries adopting AI. With patient data being as sensitive as the intricacies of a cancer diagnosis, any technological solution must rigorously address privacy considerations. The integration of AI is loaded with issues relating to data security, making strict privacy controls an essential component of AI programs.
Clinicians and patient advocacy groups are urging that AI platforms in oncology deploy a closed-system approach. This means using validated AI tools that ensure patient data is processed securely, thus preserving trust in the health care system. The development of these systems often involves close cooperation with major technology companies, whose role is to embed robust security measures into the foundation of these applications.
Key privacy strategies include:
- Closed-System AI: These systems restrict data access to a known, controlled environment, reducing the risk of breaches.
- Verified Data Sources: Ensuring that all inputs into the AI are validated and come from trusted sources increases the accuracy of outputs.
- Strict Consent Protocols: Both patients and caregivers must be made aware of how their data is used, giving them the power to make informed choices about their participation.
To further illustrate these efforts, consider the table below that outlines common strategies used to uphold data privacy in AI-assisted oncology:
| Strategy | Description |
|---|---|
| Closed-System Architecture | Limits data sharing to secured, controlled environments with no external access. |
| Data Encryption | Uses advanced encryption methods to secure sensitive patient data against unauthorized access. |
| User Consent Management | Implements clear and comprehensive consent protocols to ensure patients understand how their data is used. |
| Regular Security Audits | Conducts frequent evaluations of security measures to identify and patch vulnerabilities. |
By consistently applying these precautions, the oncology community can build greater confidence in the use of AI as a super important tool for advancing patient care.
Ethical Considerations: The Human Element in AI-Driven Health Care
With any significant technological shift, ethical concerns naturally arise. In the case of AI in oncology, critics argue that there is a risk of diminishing the human element in care. Amid the overwhelming potential benefits, the conversation must also tackle the tangled issues of trust, empathy, and the essential personal connection between patients and their providers.
Clinicians emphasize that while AI can offer data-driven insights, the final responsibility always rests with the human caregiver. This balance is critical in culture-sensitive fields like oncology, where every minor decision can have profound impacts on patient well-being.
Some of the fine points at the heart of these ethical debates include:
- Maintaining Trust: The technology should support, never replace, human judgment, preserving the integrity of patient-clinician interactions.
- Transparency in Algorithms: There is a pressing need for clear communication about how AI reaches its conclusions, to reassure patients about the small distinctions between machine-generated suggestions and human oversight.
- Responsibility and Liability: Clear lines must be drawn regarding who is accountable when AI recommendations are integrated into treatment protocols.
Ultimately, this ethical discussion is filled with tricky parts and subtle bits that require collaboration among physicians, AI developers, and patient representatives. The goal is to forge a path where advanced technology and compassionate care can coexist seamlessly.
Establishing Safe AI Practices Through Collaborative Partnerships
One central approach to addressing the nerve-racking challenges posed by AI in oncology is the formation of strategic partnerships. By teaming up with established tech giants—entities known for their prowess in data security and system management—oncology centers can harness AI in a safe, controlled manner.
These partnerships have already borne fruit in pilot programs that use closed-system AI solutions. In these programs, data privacy is safeguarded, and only validated information is used to guide intervention strategies. The collaboration ensures that the innovative power of AI is matched with tried-and-true security practices, thereby driving trustworthy outcomes for both patients and caregivers.
Characteristics of successful AI collaborations include:
- Shared Decision-Making Tools: Platforms that promote teamwork between clinicians and AI, which allow expert human judgment to remain the cornerstone of treatment decisions.
- Third-Party Partnerships: Collaborations with companies like Amazon Web Services (AWS) to implement and monitor AI functionalities while upholding strict privacy standards.
- Continuous Improvement: Regular feedback loops where clinicians assess AI recommendations and provide insights that are used to refine the algorithms.
These partnerships are vital because they bridge the gap between raw technological capability and the nuanced needs of cancer care. They ensure that the machine’s role is supportive, boosting the clinical team’s effectiveness rather than undermining the vital hands-on care provided by human experts.
Overcoming the Overwhelming Concerns: A Path Forward
Even as new AI applications promise improved clinical outcomes and administrative efficiency, there remains a nerve-racking cloud of skepticism. For many patients and caregivers, the transition to AI-supported treatment protocols is both intimidating and off-putting due to the possibility that it might diminish the personal connection found in traditional care settings.
To overcome these concerns, it is necessary to openly address the small distinctions and subtle parts of AI technology. Education and clear communication are key: patients must be informed about how AI works, what its limitations are, and how their data is protected. Healthcare providers need to take a closer look at AI’s capabilities while continuing to emphasize the human side of medicine.
Here are some actionable steps that could help ease these concerns:
- Enhanced Patient Education: Workshops, seminars, and one-on-one sessions that explain AI processes in plain language.
- Regular Feedback Sessions: Forums where patients and caregivers can share their experiences and voice concerns regarding AI in oncology care.
- Hybrid Decision-Making Models: Clinicians can use AI as a guide while making it clear that final treatment decisions are based on human judgment.
- Transparent Data Practices: Clear communication on data usage, storage, and security protocols that reassure patients their private information is managed safely.
By implementing these measures, the oncology community can help transform what might seem a confusing and overwhelming shift into a collaborative, transparent process that truly benefits patient care.
Learning from the Field: Real-World Experiences and Case Studies
Insights from leading oncology centers provide a window into how AI is already beginning to reshape patient care. For example, institutions that have implemented closed-system AI tools report notable improvements in workflow efficiency and data accuracy. These institutions have used AI to help sort through thousands of data points, furnishing clinicians with actionable insights while ensuring that sensitive patient information remains secure.
Case studies demonstrate that by delegating the more monotonous tasks to technology, clinicians can devote more of their time to personalized patient interactions—an outcome that both supports the promise of AI and addresses the concerns raised by its critics.
A brief overview of case study highlights:
- Reduced Administrative Overload: One center reported a 30% reduction in paperwork time, allowing for more dedicated patient care.
- Enhanced Treatment Accuracy: Predictive algorithms enabled early identification of potential treatment complications, leading to quicker intervention in several instances.
- Improved Patient Satisfaction: Feedback from patients indicated that streamlined processes led to a more efficient experience, even as many insisted on the irreplaceable nature of direct, personal contact.
These real-world applications underscore that while the journey to fully integrating AI in oncology care is filled with twists and turns, strategic collaboration and patient-centered practices can pave the way toward a more efficient and empathetic treatment framework.
The Future of AI in Oncology: Striking a Balance Between Innovation and Empathy
Looking ahead, the continuing evolution of AI in oncology presents a hopeful yet cautious picture. The technology is set to become a super important aspect of modern cancer care, particularly when used to support clinicians rather than substitute their judgment. As AI tools develop, the focus must remain on enhancing, not overshadowing, the human connection that is so critical in health care.
Key priorities in the near future include:
- Ongoing Provider Training: Equipping clinicians with the knowledge to strategically use AI-enhanced tools while preserving their personal touch in patient interactions.
- Adaptive Algorithm Improvement: Creating systems that learn from real-time feedback in order to minimize those confusing bits and ensure recommendations remain relevant.
- Strengthened Regulatory Guidelines: Developing clear policies that protect patient interests without stifling innovation in this rapidly evolving field.
It is essential for healthcare leaders to figure a path where the benefits of AI can be maximized while its limitations are openly acknowledged and mitigated. Balancing advanced technology with core values of empathy and personal attention will ensure that cancer care remains both innovative and human-centered.
Conclusion: Embracing AI with Eyes Wide Open
The integration of AI in oncology stands at a crossroads—one that requires careful consideration of both technological promises and the human elements of health care. Patients and caregivers are equally excited by the potential to improve administrative efficiency, personalized treatment strategies, and overall care delivery, while also remaining alert to the risk of reduced personal interaction and unanswered privacy concerns.
In our collective journey toward a future where AI supports cancer care, it is critical to manage your way through the nerve-racking details with transparency, robust training, and a firm commitment to preserving the humanness at the core of medical treatment. By partnering with trusted tech giants, prioritizing patient education, and keeping ethical considerations in constant focus, the oncology community can successfully harness AI’s power without sacrificing the key human touch that defines true health care.
As we continue to work through these challenging bits and subtle parts, one thing remains clear: embracing AI in oncology is a path filled with both promise and intricate challenges. With vigilant oversight, effective collaboration, and a steadfast commitment to ethical standards, AI can be an essential partner in the fight against cancer—one that empowers clinicians and reassures patients that technology and warm, compassionate care can indeed walk hand in hand.
Originally Post From https://www.cancernetwork.com/view/how-can-ai-be-safely-used-to-support-patients-during-cancer-treatment-
Read more about this topic at
Artificial Intelligence (AI) in SAFe
Integrating AI into Product Owner and Scrum Master Roles